Author's details
- Dr Oluwasegun Kolade.
- MBBS, FWACS, MRCS.
- Consultant Orthopaedic Surgeon Federal Medical Center Owo.
Reviewer's details
- Dr AROJURAYE Soliudeen Adebayo,
- MBBS, FWACS, FMCOrtho, FACS.
- Department of Orthopaedics, National Orthopaedic Hospital, Dala, Kano, Nigeria
- Date Uploaded: 2025-06-10
- Date Updated: 2025-12-20
Pertrochanteric and Subtrochanteric Femoral Fractures
Key Messages
- These fractures are common in the elderly and trauma victims, with rising incidence in sub-Saharan Africa due to aging, accidents, and late presentation.
- Diagnosis relies on clinical signs and imaging (X-ray, CT, MRI); classification follows AO/OTA guidelines.
- Treatment includes pain management, surgical fixation (nailing or plating), or conservative care for high-risk patients.
- Early mobilization, DVT and antibiotic prophylaxis, and rehabilitation are crucial for recovery.
Pertrochanteric and subtrochanteric fractures are common types of proximal femoral fractures, particularly among the elderly population and trauma victims. In sub-Saharan Africa, these injuries are increasingly encountered due to an aging population, motor vehicle accidents, falls from heights, and occupational injuries.
The pertrochanteric and subtrochanteric femoral fractures are fractures involving the proximal part of the femoral shaft. The pertrochanteric femoral fractures are fractures involving the greater and lesser trochanters of the femur. The subtrochanteric part of the femur is the area that is between the lesser trochanter and 5 cm below the lesser trochanter.
Epidemiology in Sub-Saharan Africa
- Increasing due to urbanization, motorization, and aging populations.
- Many rural patients present late due to travel distances, financial constraints, and reliance on traditional bone setters.
- Female sex, osteoporosis, and nutritional deficiencies (vitamin D and calcium) are contributing factors.
- HIV-related bone loss and chronic steroid use in comorbidities such as TB may increase fracture risk.
Aetiology
They are commonly seen following ground level falls in the elderly population for pertrochanteric femoral fractures.
Subtrochanteric fractures occur in low energy (in the elderly) or high energy (in young individuals) trauma.
In elderly patients, rule out pathologic or atypical femur fracture. Pathologic fracture may occur due to primary or metabolic bone disease.
Clinical Presentation
Hip pain: This usually has an acute onset following trauma. It is an antecedent in the presence of pathological fracture.
Inability to ambulate on the affected limb or raise it up.
Physical Findings may include:
- Shortening of the affected lower limb and externally rotated
- Thigh swelling or bruising.
- Deformity of the thigh
- Tenderness over the fracture site, groin, hip or upper thigh
- Neurovascular assessment.
- Rule out associated injuries, especially in polytrauma
Different Diagnosis
- Femoral neck fracture.
- Femoral shaft fracture.
Investigation
- Plain radiograph: Thigh x-ray. Anteroposterior pelvis and lateral hip X-rays. Full-length femur X-ray to exclude shaft extension. The whole extent of the thigh must be visible. Figures 1 and 2
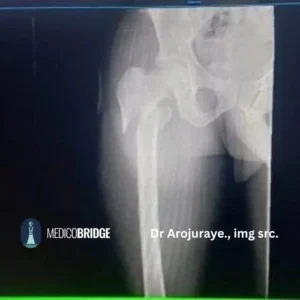
Figure 1. Pertrochanter fracture. Picture credit Dr AROJURAYE Soliudeen Adebayo.

Figure 2. Pertrochanter fracture. Picture credit Dr AROJURAYE Soliudeen Adebayo.

Figure 3 Pertrochanter fracture Picture credit Dr AROJURAYE Soliudeen Adebayo
- CT scan of the femur helps to better characterise the fracture pattern and helps in surgical planning for the patient.
- MRI: in occult hip fracture
- Blood tests: Full blood count, electrolyte urea and creatinine. Glucose checks in adults to rule out diabetes mellitus.
Classification
Pertrochanteric Fractures
- Occur between the greater and lesser trochanters.
- Usually extracapsular.
- AO/OTA classification: 31-A1 to A3.
- Russel classification
Subtrochanteric Fractures
- Occur below the lesser trochanter, up to 5 cm distally.
- Often associated with high-energy trauma in young adults or pathological fractures in elderly.
- AO/OTA classification: 32-A to 32-C.
Treatment
In major trauma, manage the patient using ATLS protocol to identify life threatening conditions in the patient and treat such conditions first.
Goals of Fracture Treatment
- Save life
- Save limb
- Restore function.
Pain Management
- Multimodal
- Parenteral analgesics
- Nerve block
- Apply skin traction which helps to reduce pain and further injury to the surrounding soft tissue especially neurovascular bundles from fracture edges.
Surgical Management
- Children < 5 years old hip spica or Gallow splint are recommended. Skin traction can be used initially to ensure adequate length is achieved and in hip spica can be applied once the fracture is sticky.
- In older children, treat with ORIF with plates and screws or TENS nailing or intramedullary nails.
- Adults subtrochanteric fractures closed or open reduction with proximal femoral nail or proximal locked femoral plate plus screw or dynamic hip screw.
NB- The choice of implants depends on the fracture pattern and surgeon’s preference.
- Non-operative may be indicated in patients who are bedridden or non-ambulatory with many co-morbidities because they are high anaesthetic risk patients thus poor candidates for anaesthesia or high-risk patients or lack of surgical access. Skeletal traction or skin traction, analgesia, and nursing care. Risk of complications: pressure sores, DVT, pulmonary infections.
Pertrochanteric Fracture Management
Indications for conservative non-operative management include non-ambulatory patients, high risk for perioperative mortality.
Operative Treatment (Figures 4 and 5)
- Closed reduction and intramedullary nailing.
- Open reduction and internal fixation with proximal femur locking plates, sliding hip compression or angle blade plate.
- Arthroplasty is indicated as a salvage for failed internal fixation or in severe comminution of fracture or a preexisting hip osteoarthritis.

Figure 4 Pertrochanteric fracture treated with DHS Picture credit Dr AROJURAYE Soliudeen Adebayo.

Figure 5: Post op plan radiograph who had CRIF with PFN on account of reverse oblique. Picture credit Dr AROJURAYE Soliudeen Adebayo.
Postoperative Care
- Early mobilization (within 48 hours) reduces morbidity.
- DVT prophylaxis: low-molecular-weight heparin (where available) or mechanical methods.
- Antibiotic prophylaxis for surgical patients.
- Calcium and vitamin D supplementation for all elderly fracture patients.
Rehabilitation and Follow-up
- Physiotherapy services are often limited—community-based rehab programs are essential.
- Encourage caregiver involvement and use of walking aids.
- Monitor for implant failure, malunion, or infection.
Complications
- Non-union or malunion, especially in poorly reduced subtrochanteric fractures.
- Deep infections, particularly in settings with inadequate sterile conditions.
- Implant failure if poor technique or inferior implant quality.
- Avascular necrosis is rare in extracapsular fractures but must be considered.
Public Health and Contextual Considerations
- Lack of trained orthopedic surgeons at the district level.
- The cost of surgery and implants are often unaffordable to patients without subsidies or insurance.
- Cultural preferences for traditional bone-setting delay appropriate care.
- Encourage task-shifting (training general surgeons in basic ortho procedures).
- Advocacy for orthopedic implant donations and surgical training.
Prevention Strategies
- Fall prevention in elderly (home safety, vision checks, balance training).
- Nutritional programs to address osteoporosis.
- Calcium + Vitamin D supplementation in high-risk populations.
- Public education on avoiding delays in hospital presentation after trauma.
Key Takeaways
- The management of pertrochaneric and subtrochanteric fractures should be patient centered depending on their condition, the type of fracture and previous comorbidities.
- Timely and appropriate management of pertrochanteric and subtrochanteric fractures can restore function and prevent long-term disability.
- In sub-Saharan Africa, challenges include delayed presentation, resource constraints, and limited surgical capacity.
- Strengthening trauma systems, investing in training, and improving access to implants are crucial for improving outcomes.
Subtrochanteric Fracture
Patient: A 68-year-old female presented to the emergency department after slipping and falling at home while fetching water. She was unable to stand or bear weight on her left leg.
Examination:
- Left leg shortened and externally rotated
- Tenderness and swelling over the upper thigh
- No neurovascular deficits
Imaging:
- X-ray revealed a transverse subtrochanteric fracture of the left femur.
Management:
- Admitted and stabilized
- Surgery performed using intramedullary nailing
- Started physiotherapy on day 2 post-op
- Discharged on day 5 with follow-up planned for 2 weeks
Outcome: Patient recovering well with assisted ambulation and no postoperative complications.
Related Topics
- AO/OTA Fracture and Dislocation Classification Compendium-2018 Available at https://www.aofoundation.org/trauma/clinical-library-and-tools/journals-and-publications/classification Accessed June 2025.
- Gakuu LN, et al. “Management of Femoral Fractures in Low-Resource Settings.” E. Afr Med J, 2020.
- WHO. Essential Trauma Care Guidelines, 2004.
- Parker MJ, Handoll HH. “Surgical Interventions for Hip Fractures in Adults.” Cochrane Database, 2022.
- Ogunlade SO et al. “Femoral Fractures in Nigeria: Patterns and Surgical Options.” West Afr J Med, 2019.

More topics to explore
Author's details
Reviewer's details
Pertrochanteric and Subtrochanteric Femoral Fractures
- Background
- Symptoms
- Clinical findings
- Differential diagnosis
- Investigations
- Treatment
- Follow-up
- Prevention and control
- Further readings
Pertrochanteric and subtrochanteric fractures are common types of proximal femoral fractures, particularly among the elderly population and trauma victims. In sub-Saharan Africa, these injuries are increasingly encountered due to an aging population, motor vehicle accidents, falls from heights, and occupational injuries.
The pertrochanteric and subtrochanteric femoral fractures are fractures involving the proximal part of the femoral shaft. The pertrochanteric femoral fractures are fractures involving the greater and lesser trochanters of the femur. The subtrochanteric part of the femur is the area that is between the lesser trochanter and 5 cm below the lesser trochanter.
- AO/OTA Fracture and Dislocation Classification Compendium-2018 Available at https://www.aofoundation.org/trauma/clinical-library-and-tools/journals-and-publications/classification Accessed June 2025.
- Gakuu LN, et al. “Management of Femoral Fractures in Low-Resource Settings.” E. Afr Med J, 2020.
- WHO. Essential Trauma Care Guidelines, 2004.
- Parker MJ, Handoll HH. “Surgical Interventions for Hip Fractures in Adults.” Cochrane Database, 2022.
- Ogunlade SO et al. “Femoral Fractures in Nigeria: Patterns and Surgical Options.” West Afr J Med, 2019.

Content
Author's details
Reviewer's details
Pertrochanteric and Subtrochanteric Femoral Fractures
Background
Pertrochanteric and subtrochanteric fractures are common types of proximal femoral fractures, particularly among the elderly population and trauma victims. In sub-Saharan Africa, these injuries are increasingly encountered due to an aging population, motor vehicle accidents, falls from heights, and occupational injuries.
The pertrochanteric and subtrochanteric femoral fractures are fractures involving the proximal part of the femoral shaft. The pertrochanteric femoral fractures are fractures involving the greater and lesser trochanters of the femur. The subtrochanteric part of the femur is the area that is between the lesser trochanter and 5 cm below the lesser trochanter.
Further readings
- AO/OTA Fracture and Dislocation Classification Compendium-2018 Available at https://www.aofoundation.org/trauma/clinical-library-and-tools/journals-and-publications/classification Accessed June 2025.
- Gakuu LN, et al. “Management of Femoral Fractures in Low-Resource Settings.” E. Afr Med J, 2020.
- WHO. Essential Trauma Care Guidelines, 2004.
- Parker MJ, Handoll HH. “Surgical Interventions for Hip Fractures in Adults.” Cochrane Database, 2022.
- Ogunlade SO et al. “Femoral Fractures in Nigeria: Patterns and Surgical Options.” West Afr J Med, 2019.
Advertisement

