Author's details
- Taofik Ogunkunle
- MBBS, FWACP, FMCPaed, MPH
- Consultant Paediatrician, Dalhatu Araf Specialist Hospital, Lafia, Senior Clinical Research Scientist, International Foundation Against Infectious Disease in Nigeria (IFAIN)
Reviewer's details
- Prof Omotayo Adesiyun
- MBBS, FMCPaed, FESPE
- Department of Paediatrics, University of Ilorin/ University of Ilorin Teaching Hospital, Ilorin
- Date Uploaded: 2024-12-02
- Date Updated: 2025-12-20
Meconium-Staining of the Amniotic Fluid and its Consequences
Key Messages
- Meconium-stained amniotic fluid (MSAF) is common at term and can signal fetal distress.
- The main risk is meconium aspiration syndrome (MAS), causing newborn respiratory distress and possible severe complications.
- Diagnosis is clinical, supported by imaging and oxygen monitoring.
- Treatment is supportive; routine suctioning is not recommended.
Meconium is the earliest stool of an infant. It is a viscous, dark-green substance composed of water, intestinal epithelial cells, lanugo, mucus, and intestinal secretions (e.g., bile). Meconium-stained amniotic fluid (MSAF) occurs when a fetus passes meconium into the amniotic fluid. It is found in 10 – 15% of births and usually occurs in term or post-term infants. Incidences tend to increase after term and could be as high as o 15 – 20% after 40 weeks.(1,2)
Meconium-stained amniotic fluid often indicates fetal distress but is also seen in normal-term deliveries. Risk factors for MASF include primiparity, prolonged rupture of fetal membranes, prolonged labour, obstructed labour, advanced gestational age, preeclampsia, and non-reassuring fetal heart rate.(3–5)
The presence of meconium in the amniotic fluid could have some consequences which include:
- May increase the risk of perinatal bacterial infection – Meconium may enhance the growth of bacteria in amniotic fluid by inhibiting the bacteriostatic properties of amniotic fluid. Bacterial endotoxins and bacteria have been frequently recovered from amniotic fluid stained with meconium.(6)
- Integument staining and irritation – It causes skin irritation and hence increases the risk of erythema toxicum, a benign self-limiting skin eruption appearing within the first week of life, and it typically improves within 1 – 2 weeks. Also, it stains the nails and skin of the newborn.(2)
- Aspiration of meconium-stained amniotic fluid – Meconium aspiration develops in about 5% of newborns with MSAF and it is referred to as meconium aspiration syndrome (MAS). It is the most severe consequence of meconium staining of amniotic fluid with 30% requiring mechanical ventilation and about 5% dying.(1) Death rates could, however, be higher in resource-poor settings with minimal facilities for respiratory support. Once aspirated, meconium-staining amniotic fluid could induce respiratory pathology through diverse means (summarized below) culminating in ventilation-perfusion mismatch, hypoxaemia, acidosis and respiratory distress. Affected newborns often develop profound respiratory distress shortly after birth.
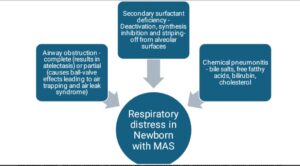
Figure credit: The Author
4. Increased risk of persistent pulmonary hypertension of newborns (PPHN) – Persistent hypoxaemia, hypercarbia and acidosis in babies with MAS could result in pulmonary vasoconstriction, eventual thickening of the pulmonary vessels and persistent elevation in pulmonary vascular resistance. The resultant increased pulmonary vascular pressure leads right to left shunt across the foramen ovale and/or ductus arteriosus.
Amniotic fluid is greenish at delivery due to the presence of meconium. The infant often presents with stained skin, nails, and umbilical cord. Infants delivered through MSAF might be vigorous i.e., having good tone and respiratory effort or non-vigorous with hypotonia. Bradycardia and poor respiratory efforts and muscle tone. In the latter, a history of antepartum or intrapartum fetal distress is frequently present and the infant has a high risk of MAS.(1)
Babies with MAS develop respiratory distress shortly after birth which worsens over the ensuing 48 hours. Features of respiratory distress include fast breathing, flaring of ala nasi, cyanosis, grunting, and intercostal retractions. The condition usually improves within 72 hours, but when the course of respiratory distress is severe enough to warrant assisted ventilation, the risk of mortality is usually high. If untreated, distress can progress to respiratory failure and death within 24 hours of onset.(2)
Infants with MAS are usually sick. Clinically, affected infants would have tachypnoea or bradypnoea terminally when exhausted which would suggest impending respiratory failure. Also, there is evidence of increased work of breathing such as chest recessions and retractions. The chest could be barrel-shaped which would suggest associated complications such as pneumothorax. Diffuse rales and rhonchi might be demonstrable on auscultation in some cases while there could be differential air entry due to airway obstructions.(1,2) Babies with MAS can present with features and complications of intrapartum asphyxia (e.g., hypoxic encephalopathy), which was primarily responsible for fetal distress and in-utero passage of meconium.
Differential diagnoses include other causes of respiratory distress in neonates, such as pneumonia, sepsis, or congenital cardiac malformations.
Chest X-rays could be ordered. The typical chest radiograph is characterized by patchy infiltrates and coarse streaking of both lung fields with variable aeration. Increased anteroposterior diameter and flattening of the diaphragm may be observed if there is air-trapping and air-leak syndrome.
Pulse oximetry is done to determine oxygen saturation. This is crucial at presentation and subsequently to monitor improvement or deterioration. Also, Echocardiography could be done to exclude congenital cardiac anomalies or to diagnose PPHN. A normal chest roentgenogram in an infant with severe hypoxemia and no cardiac malformation suggests the diagnosis of pulmonary hypertension.
Other investigations such as complete blood count, acute phase markers of bacterial infections e.g., C-Reactive protein or procalcitonin and blood culture might be required if sepsis is a serious consideration.
The initial management of a newborn delivered through MSAF is the immediate assessment of the newborn’s airway, breathing, and circulation. It should be noted that routine intrapartum suctioning or intubation to aspirate the lungs of all infants born through meconium-stained fluid is not effective in reducing the MAS or other major adverse outcomes and is currently not recommended.(7)
A vigorous infant delivered through MSAF may require no more than a gentle clearing of meconium from the mouth and nose with a bulb syringe and can be observed further for signs of deterioration while maintaining skin-to-skin contact with the mother. A non-vigorous infant on the other hand should be moved to a resuscitaire (radiant warmer) and be resuscitated as per the neonatal resuscitation guidelines.(7) The baseline risk of pneumothorax must always be borne when administering bag and mask ventilation.
Treatment of the MAS includes supportive care and standard management for respiratory distress.
- Continuous Positive Airway Pressure (CPAP) is beneficial especially when there is increased work of breathing.
- Administration of exogenous surfactant – could reduce the need for mechanical ventilation if available and affordable
- Administration of inhaled Nitric oxide (iNO) – It could reduce the need for mechanical ventilation if available and affordable. The optimal starting dose is 20 ppm, and the dose can be weaned to 5 ppm after 6 – 24 hours of therapy.
- Conventional mechanical ventilation – This is required in infants with hypoxemic respiratory failure, or pulmonary hypertension.
- Extracorporeal Membrane Oxygenation (ECMO) – Patients with MAS that are refractory to conventional mechanical ventilation.
- Supportive care – Hypoglycaemia (glucose level <50mg/dl), if present should be treated with 200mg/dl of dextrose administered as IV bolus. Intravenous fluid should be provided to infants with MAS at a rate that will provide maintenance glucose concentration of 6 – 8 mg/kg/hour. Antibiotics may be used as prophylaxis.
Most babies delivered through MSAF will not develop serious respiratory symptoms and most infants with meconium aspiration will develop mild symptoms and will recover completely. The outcome of a newborn with MAF is dependent on the severity of the symptoms, presence of other organ dysfunctions e.g., hypoxic encephalopathy, timeliness and accessibility to respiratory support and care. Mortality is generally higher with delayed presentation and care in settings with limited capacity for respiratory support as well as in the presence of multiple organ dysfunction. Also, severely affected infants are at risk of dying while survivors are at risk of developing reactive airway disease or neurodevelopmental delays related to hypoxaemia. Tachypnea may persist for many days or even several weeks.
Prevention strategies of MAS focus on monitoring fetal distress and timely delivery. This involves rapid identification of fetal distress and initiation of prompt delivery in the presence of late fetal heart rate deceleration or poor beat-to-beat fetal heart rate variability. In cases of known MSAF, careful monitoring during labour and immediate neonatal care are crucial to minimizing complications.
Meconium-staining of the amniotic fluid in sub-Saharan Africa is associated with an increased risk of neonatal complications, including meconium aspiration syndrome, respiratory distress, and perinatal asphyxia. Limited access to advanced neonatal care and monitoring heightens these risks. Prompt identification, careful fetal monitoring, and timely delivery in facilities with neonatal resuscitation capabilities are crucial to reducing adverse outcomes and improving neonatal survival in the region.
A male newborn delivered in the 40th week of pregnancy by emergency C-section following a
prolonged obstructed labour. Maternal history was positive for pregnancy-induced hypertension and prolonged rupture of membrane, but the remainder of the pregnancy was uneventful. Amniotic fluid was greenish, and the baby was limp with poor respiratory efforts, cyanosis and bradycardia. The airway was cleared of copious meconium-laden amniotic fluid and
cardiopulmonary resuscitation started immediately. Baby improved subsequently with regular breathing, improved tone and heart rate. He however had chest retractions and suboptimal oxygen saturation (80%). Chest X-ray showed patchy infiltrates and coarse streaking of both lung fields with variable aeration. He was subsequently commenced on continuous positive
airway pressure (CPAP) and maintenance intravenous fluid.
- Ambalavanan N, Carlo AW. Meconium Aspiration. In: Kliegman MR, Staton FB, St Geme III WJ, Schor FN, Behrman ER, editors. Nelson Textbook of Pediatrics. 20th ed. Philadelphia: Elsevier; 2016. p. 859–62.
- Okagua J, Igbagiri F, Oruamabo SR. Meconium staining of the amniotic fluid and its consequences on the Newborn. In: Azubuike CJ, Nkanginieme EOK, Nte RA, Adedoyin TO, editors. Paediatrics and Child Health in a Tropical Region. 3rd ed. Lagos: Educational Printing and Publishing; 2016. p. 352–6.
- David AN, Njokanma OF, Iroha E. Incidence of and factors associated with meconium staining of the amniotic fluid in a Nigerian University Teaching Hospital. J Obstet Gynaecol. 2006 Aug 1;26(6):518–20.
- Silassie RG/, Gebretsadik W, Degefa N, Getahun D, Kassie N. Determinants of Meconium-Stained Amniotic Fluid at Hadiya Zone Hospitals, Southern Ethiopia; Unmatched Case-Control Study. International Journal of Women’s Health . 2022;14:1351–60.
- Addisu D, Asres A, Gedefaw G, Asmer S. Prevalence of meconium-stained amniotic fluid and its associated factors among women who gave birth at term in Felege Hiwot comprehensive specialized referral hospital, North West Ethiopia: A facility based cross-sectional study. BMC Pregnancy Childbirth. 2018 Oct 30;18(1).
- Romero R, Yoon BH, Chaemsaithong P, Cortez J, Park CW, Gonzalez R, et al. Bacteria and endotoxin in meconium-stained amniotic fluid at term: could intra-amniotic infection cause meconium passage? J Matern Fetal Neonatal Med. 2014;27(8):775.
- Delivery of a Newborn with Meconium-Stained Amniotic Fluid | ACOG [Internet]. [cited 2024 Jun 18]. Available from: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/03/delivery-of-a-newborn-with-meconium-stained-amniotic-fluid

Author's details
Reviewer's details
Meconium-Staining of the Amniotic Fluid and its Consequences
- Background
- Symptoms
- Clinical findings
- Differential diagnosis
- Investigations
- Treatment
- Follow-up
- Prevention and control
- Further readings
Meconium is the earliest stool of an infant. It is a viscous, dark-green substance composed of water, intestinal epithelial cells, lanugo, mucus, and intestinal secretions (e.g., bile). Meconium-stained amniotic fluid (MSAF) occurs when a fetus passes meconium into the amniotic fluid. It is found in 10 – 15% of births and usually occurs in term or post-term infants. Incidences tend to increase after term and could be as high as o 15 – 20% after 40 weeks.(1,2)
Meconium-stained amniotic fluid often indicates fetal distress but is also seen in normal-term deliveries. Risk factors for MASF include primiparity, prolonged rupture of fetal membranes, prolonged labour, obstructed labour, advanced gestational age, preeclampsia, and non-reassuring fetal heart rate.(3–5)
- Ambalavanan N, Carlo AW. Meconium Aspiration. In: Kliegman MR, Staton FB, St Geme III WJ, Schor FN, Behrman ER, editors. Nelson Textbook of Pediatrics. 20th ed. Philadelphia: Elsevier; 2016. p. 859–62.
- Okagua J, Igbagiri F, Oruamabo SR. Meconium staining of the amniotic fluid and its consequences on the Newborn. In: Azubuike CJ, Nkanginieme EOK, Nte RA, Adedoyin TO, editors. Paediatrics and Child Health in a Tropical Region. 3rd ed. Lagos: Educational Printing and Publishing; 2016. p. 352–6.
- David AN, Njokanma OF, Iroha E. Incidence of and factors associated with meconium staining of the amniotic fluid in a Nigerian University Teaching Hospital. J Obstet Gynaecol. 2006 Aug 1;26(6):518–20.
- Silassie RG/, Gebretsadik W, Degefa N, Getahun D, Kassie N. Determinants of Meconium-Stained Amniotic Fluid at Hadiya Zone Hospitals, Southern Ethiopia; Unmatched Case-Control Study. International Journal of Women’s Health . 2022;14:1351–60.
- Addisu D, Asres A, Gedefaw G, Asmer S. Prevalence of meconium-stained amniotic fluid and its associated factors among women who gave birth at term in Felege Hiwot comprehensive specialized referral hospital, North West Ethiopia: A facility based cross-sectional study. BMC Pregnancy Childbirth. 2018 Oct 30;18(1).
- Romero R, Yoon BH, Chaemsaithong P, Cortez J, Park CW, Gonzalez R, et al. Bacteria and endotoxin in meconium-stained amniotic fluid at term: could intra-amniotic infection cause meconium passage? J Matern Fetal Neonatal Med. 2014;27(8):775.
- Delivery of a Newborn with Meconium-Stained Amniotic Fluid | ACOG [Internet]. [cited 2024 Jun 18]. Available from: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/03/delivery-of-a-newborn-with-meconium-stained-amniotic-fluid

Content
Author's details
Reviewer's details
Meconium-Staining of the Amniotic Fluid and its Consequences
Background
Meconium is the earliest stool of an infant. It is a viscous, dark-green substance composed of water, intestinal epithelial cells, lanugo, mucus, and intestinal secretions (e.g., bile). Meconium-stained amniotic fluid (MSAF) occurs when a fetus passes meconium into the amniotic fluid. It is found in 10 – 15% of births and usually occurs in term or post-term infants. Incidences tend to increase after term and could be as high as o 15 – 20% after 40 weeks.(1,2)
Meconium-stained amniotic fluid often indicates fetal distress but is also seen in normal-term deliveries. Risk factors for MASF include primiparity, prolonged rupture of fetal membranes, prolonged labour, obstructed labour, advanced gestational age, preeclampsia, and non-reassuring fetal heart rate.(3–5)
Further readings
- Ambalavanan N, Carlo AW. Meconium Aspiration. In: Kliegman MR, Staton FB, St Geme III WJ, Schor FN, Behrman ER, editors. Nelson Textbook of Pediatrics. 20th ed. Philadelphia: Elsevier; 2016. p. 859–62.
- Okagua J, Igbagiri F, Oruamabo SR. Meconium staining of the amniotic fluid and its consequences on the Newborn. In: Azubuike CJ, Nkanginieme EOK, Nte RA, Adedoyin TO, editors. Paediatrics and Child Health in a Tropical Region. 3rd ed. Lagos: Educational Printing and Publishing; 2016. p. 352–6.
- David AN, Njokanma OF, Iroha E. Incidence of and factors associated with meconium staining of the amniotic fluid in a Nigerian University Teaching Hospital. J Obstet Gynaecol. 2006 Aug 1;26(6):518–20.
- Silassie RG/, Gebretsadik W, Degefa N, Getahun D, Kassie N. Determinants of Meconium-Stained Amniotic Fluid at Hadiya Zone Hospitals, Southern Ethiopia; Unmatched Case-Control Study. International Journal of Women’s Health . 2022;14:1351–60.
- Addisu D, Asres A, Gedefaw G, Asmer S. Prevalence of meconium-stained amniotic fluid and its associated factors among women who gave birth at term in Felege Hiwot comprehensive specialized referral hospital, North West Ethiopia: A facility based cross-sectional study. BMC Pregnancy Childbirth. 2018 Oct 30;18(1).
- Romero R, Yoon BH, Chaemsaithong P, Cortez J, Park CW, Gonzalez R, et al. Bacteria and endotoxin in meconium-stained amniotic fluid at term: could intra-amniotic infection cause meconium passage? J Matern Fetal Neonatal Med. 2014;27(8):775.
- Delivery of a Newborn with Meconium-Stained Amniotic Fluid | ACOG [Internet]. [cited 2024 Jun 18]. Available from: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/03/delivery-of-a-newborn-with-meconium-stained-amniotic-fluid
Advertisement

