Author's details
- Dr Hauwa Umar Mustapha
- MBBS, MWACP in paediatrics, Senior Registrar
- Aminu Kano Teaching Hospital, Kano.
Reviewer's details
- Dr Afolayan Folake Moriliat
- (MBBS, MSc Tropical Pediatrics, FMCPaed)
- Consultant paediatrician at Kwara State Teaching Hospital, Ilorin.
- Date Uploaded: 2024-12-14
- Date Updated: 2025-02-04
Inflammatory Oncologic Emergencies in Pediatrics
Key Messages
They are life-threatening complications in children with cancer, caused by an excessive inflammatory response. These emergencies occur due to the rapid release of pro-inflammatory cytokines, often triggered by infections, cancer therapies, or the cancer itself. Examples include mucositis, typhilitis, haemorrhagic cystitis, both of which can result in systemic inflammation, multi-organ failure, and require immediate medical intervention.
This affects all mucous membrane (oral to anus). Oral mucositis is the most common. Presenta 5-10days following chemotherapy. Mucositis is caused by direct damage of mucosal lining by chemotherapeutic agents or secondary invasion by micro-organisms.
Clinical Presentation(figure 1)
• Burning oral pain.
• Erythema and ulceration.
• Difficulty eating, drinking, talking.
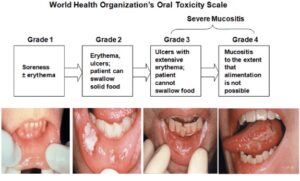
Figure 1 Mucositis. Source: Radiation induced mucositis from Osama et.al.
Diagnosis of mucositis is based on clinical judgement. Oral swab for microscopy, culture and sensitivity should be also taken.
TREATMENT
• Oral debridement eg alcohol help dislodge dried secretion.
• Oral decontamination with antibiotic and antifungal rinsing.
• Pain management.
• Prophylaxis with use of ice chip cryotherapy.
• Low level laser therapy.
This is neutropenic enterocolitis. Ranging from inflammation to necrosis or perforation. It is mostly seen in the ileocaecum. Mortality can be 100% if not noticed early
CLINICAL FEATURES
• Fever
• Diarrhoea
• Melena
• Abdominal pain
INVESTIGATION
• Abdominal ultrasound
• Abdominal CT-scan
TREATMENT
• Keep child on NPO
• IVF maintenance
• Use of broad-spectrum antibiotics
• Emergency surgical consultation.
INTRODUCTION
This is inflammation of bladder mucosa with oedema and ulceration causing haematuria. Caused by metabolites of cyclophosphamide and Ifosfamide especially acrolein. Acrolein is excreted in urine – it causes oedema, inflammation and necrosis of transitional epithelium with increased contact (Figure 2)
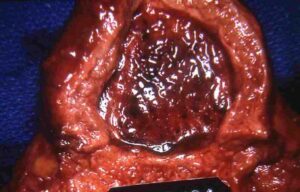
Figure 2: Haemorrhagic CystisImage source: slideshare. Minarcik robbins 2013_ch21-lower_ut
Treatment of Cystitis
• Hyperhydration and continuous bladder irrigation.
• Suprapubic catheterization.
• Platelet transfusion.
• Local instillation of prostaglandin E1, • Alum, Silver nitrate or formalin.
• Bladder resection if intractable.
• Use of Mercapto-ethane sulfonate (mesna) which binds the irritative metabolite, acrolein to produce non-toxic thio-ethers.
Oncological emergencies in children, particularly inflammatory and infection-related, pose a significant risk in sub-Saharan Africa due to limited healthcare resources, late diagnosis, and the high burden of infections. Children with cancer often have weakened immune systems due to the disease or its treatment (like chemotherapy), making them highly vulnerable to severe infections.
Effective management of these emergencies requires early detection, access to antibiotics, fluids, and supportive care, as well as timely referral to specialized centers when needed. Strengthening healthcare infrastructure, improving infection control measures, and increasing awareness in both families and healthcare providers are critical to improving outcomes for pediatric oncology patients in sub-Saharan Africa.
A 7-year-old boy undergoing chemotherapy for leukemia developed symptoms of cystitis, including pain while urinating, frequent urination, and lower abdominal discomfort. His urine appeared cloudy with occasional blood, and a urine test confirmed the presence of blood and increased white blood cells. The boy was diagnosed with hemorrhagic cystitis, a known side effect of certain chemotherapy drugs, particularly cyclophosphamide.
Treatment included increased fluid intake, pain relief, and adjustments to his chemotherapy regimen to protect the bladder. The child’s symptoms gradually improved with supportive care, and he continued his cancer treatment under close monitoring.
1. Nelson’s textbook of pediatrics 21st edition by Kleigman, Behrman, Jenson and Stanton
2. Principles and practice of pediatric oncology 4th edition by Philip.A. Pizzo and David.G. Poplack
3. Williams Haematology,6th edition,by Ernest Beutler M.D,etal.
4. Zinner SH. Changing epidemiology of infections in patients with neutropenia and cancer: emphasis on gram-positive and resistant bacteria. Clin Infect Dis.1999;29(3):490–4.
5. Melendez E, Harper MB. Risk of serious bacterial infection in isolated and unsuspected neutropenia. Acad Emerg Med. 2010;17(2):163–7.
6. Moon JM, Chun BJ. Predicting the complicated neutropenic fever in the emergency department. Emerg Med J. 2009;26(11):802–6.
7. Roland T. Skeel- Handbook of cancer chemotherapy
8. Rheingold & Lange, “Oncologic Emergencies”, in Principles & Practice of Pediatric Oncology, eds Pizzo, Poplack.
9. Nazemi Emerg Med Clin N Am 27 (2009) 477–495.

More topics to explore
Author's details
Reviewer's details
Inflammatory Oncologic Emergencies in Pediatrics
- Background
- Symptoms
- Clinical findings
- Differential diagnosis
- Investigations
- Treatment
- Follow-up
- Prevention and control
- Further readings
They are life-threatening complications in children with cancer, caused by an excessive inflammatory response. These emergencies occur due to the rapid release of pro-inflammatory cytokines, often triggered by infections, cancer therapies, or the cancer itself. Examples include mucositis, typhilitis, haemorrhagic cystitis, both of which can result in systemic inflammation, multi-organ failure, and require immediate medical intervention.
1. Nelson’s textbook of pediatrics 21st edition by Kleigman, Behrman, Jenson and Stanton
2. Principles and practice of pediatric oncology 4th edition by Philip.A. Pizzo and David.G. Poplack
3. Williams Haematology,6th edition,by Ernest Beutler M.D,etal.
4. Zinner SH. Changing epidemiology of infections in patients with neutropenia and cancer: emphasis on gram-positive and resistant bacteria. Clin Infect Dis.1999;29(3):490–4.
5. Melendez E, Harper MB. Risk of serious bacterial infection in isolated and unsuspected neutropenia. Acad Emerg Med. 2010;17(2):163–7.
6. Moon JM, Chun BJ. Predicting the complicated neutropenic fever in the emergency department. Emerg Med J. 2009;26(11):802–6.
7. Roland T. Skeel- Handbook of cancer chemotherapy
8. Rheingold & Lange, “Oncologic Emergencies”, in Principles & Practice of Pediatric Oncology, eds Pizzo, Poplack.
9. Nazemi Emerg Med Clin N Am 27 (2009) 477–495.

Content
Author's details
Reviewer's details
Inflammatory Oncologic Emergencies in Pediatrics
Background
They are life-threatening complications in children with cancer, caused by an excessive inflammatory response. These emergencies occur due to the rapid release of pro-inflammatory cytokines, often triggered by infections, cancer therapies, or the cancer itself. Examples include mucositis, typhilitis, haemorrhagic cystitis, both of which can result in systemic inflammation, multi-organ failure, and require immediate medical intervention.
Further readings
1. Nelson’s textbook of pediatrics 21st edition by Kleigman, Behrman, Jenson and Stanton
2. Principles and practice of pediatric oncology 4th edition by Philip.A. Pizzo and David.G. Poplack
3. Williams Haematology,6th edition,by Ernest Beutler M.D,etal.
4. Zinner SH. Changing epidemiology of infections in patients with neutropenia and cancer: emphasis on gram-positive and resistant bacteria. Clin Infect Dis.1999;29(3):490–4.
5. Melendez E, Harper MB. Risk of serious bacterial infection in isolated and unsuspected neutropenia. Acad Emerg Med. 2010;17(2):163–7.
6. Moon JM, Chun BJ. Predicting the complicated neutropenic fever in the emergency department. Emerg Med J. 2009;26(11):802–6.
7. Roland T. Skeel- Handbook of cancer chemotherapy
8. Rheingold & Lange, “Oncologic Emergencies”, in Principles & Practice of Pediatric Oncology, eds Pizzo, Poplack.
9. Nazemi Emerg Med Clin N Am 27 (2009) 477–495.
Advertisement

