Author's details
- Dr. Oluwasegun Kolade
- MBBS, FWACS, MRCS.
- Consultant Orthopaedic Surgeon Federal Medical Center Owo
Reviewer's details
- Dr. AROJURAYE Soliudeen Adebayo
- MBBS, FWACS, FMCOrtho, FACS.
- Department of Orthopaedics, National Orthopaedic Hospital, Dala, Kano, Nigeria Hip Dislocation
- Date Uploaded: 2025-01-22
- Date Updated: 2025-12-20
Hip Dislocation
Key Messages
- Hip dislocation is an orthopedic emergency; mostly caused by high-energy trauma and requires immediate reduction to prevent joint damage.
- Posterior dislocation accounts for 90% of cases; diagnosis is confirmed by pelvic radiograph, and treatment involves closed or open reduction depending on complexity.
- Prompt neurovascular assessment and management of life-threatening injuries are essential.
- Prognosis is best when reduction occurs within 12 hours, delayed or inadequate care increases risk of complications.
The hip joint is a ball and socket type of synovial joint. Dislocation is an orthopaedic emergency as immediate reduction is needed to prevent destruction of the joint. Hip dislocation needs a high amount of energy to occur. Diagnosis can be confirmed with pelvic radiograph. Treatment involves emergency reduction of the dislocation, check stability after reduction and do a control radiograph to confirm reduction and rule out other any associated fracture. Hip dislocation can affect both native and artificial joints (total hip replacement).
Hip dislocation is the second most common dislocation after shoulder in the major joints.
Hip dislocation usually follows high energy trauma in road traffic injury, falls, industrial and sport injuries
Classification of Hip Dislocation
A). Anatomical Classification:
a). Posterior dislocation occurs in 90 % of cases.
b). Anterior dislocation
B). Severity or Extent of Injury
a). Simple: only dislocation of the hip with no fracture.
b). Complex Dislocation: Fracture dislocation. Hip dislocation with associated ipsilateral fractures of the acetabulum, femoral head or neck.
C). Radiological Classification: Thompson-Epstein Classification used for posterior hip dislocation.
Patient usually present following an injury. They complain of pain or deformity of the affected hip and inability to bear weight in the lower extremity. The Advanced Trauma Life Saving protocol should use to attend to them due to high energy trauma and to look out for any life-threatening injuries in the patient which should be treated first. The neurovascular examination of the limb is important as sciatic nerve, or its branches injury can occur.
In posterior hip dislocation, the patient’s hip flexed and adducted prior to injury usually following dashboard injury. The patient presents with a shortened lower limb on the affected side, the hip and leg are flexed, adducted and internally rotated.
In anterior hip dislocation
Position of the hip at injury hip in abduction and external rotated. At presentation, hip appears in flexion abduction and external rotation.
Pelvic Radiograph: This confirms the diagnosis (figures 1 & 2) and if associated fractures. It is important that a pre-reduction radiograph is obtained to rule out associated fracture in complex dislocation and medicolegal issues. A post reduction x-ray is essential to rule out fracture that could occur during reduction or not seen on pre-reduction.

Figure 1: Pelvic plain radiograph of a patient with anterior hip dislocation

Figure 2: Pelvic plain radiograph of a patient with posterior hip dislocation
Figures 1 & 2. Source: National orthopaedic hospital, Dala Kano
CT-scan of the pelvis may be necessary in fracture dislocation to characterise the associated fracture.
Identify and treat promptly life-threatening condition is crucial. The goal of treatment is to save life, limb and restore function.
The treatment of hip dislocation is immediate reduction as soon as possible. Reduction is under general anaesthesia (GA). Analgesics and muscle relaxants could be an alternative where there is unavailability of GA or no facility for it.
There are various methods of hip dislocation reduction (Figures 3-7) e.g. Simple longitudinal traction hip reduction, Allis, Bigelow, Captain Morgan, Whistler or Stimson techniques. A rule of thumb is to learn a technique and know how to apply it well.
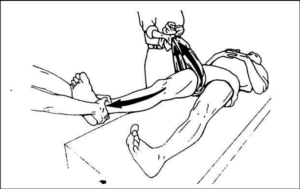
Figure 3 Simple Longitudinal traction hip reduction method. https://www.researchgate.net/figure/Figure-Simple-longitudinal-traction-hip-reduction-method_fig1_291006536.

Figure 4. Bigelow Reduction. https://pmc.ncbi.nlm.nih.gov/articles/PMC4821229/.

Figure 5. Allis method for hip reduction. https://www.semanticscholar.org/paper/Table-56-1-Structures-within-Compartments-of-the-Murray/d522ca511bd6b33266ffb487d89009d02683cdd2.
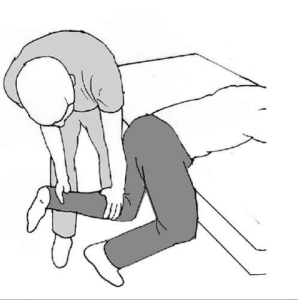
Figure 6. Stimson gravity maneuver. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC4821229/

Figure 7. Captain Morgan hip reduction. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC4821229/.
Assess hip stability after reduction by moving the joint in different directions. For simple dislocation, follow with protected weight bearing in 4-6 weeks.
This may be needed if close reduction fails or there is small fracture chip in the joint space to remove it. Approaches depends on type of dislocation.
Anterior dislocation - anterior approach
Posterior dislocation - the posterior approach
Repair of other injuries should be done at the same time.
This is good in most simple dislocation with prompt treatment. Best prognosis is achieved when reduction is done within 12 hours post injury. Prognosis also depends on the amount of energy to the hip and associated injury.
Hip dislocation in low-resource settings presents challenges due to limited access to advanced medical care and imaging. Prompt diagnosis is often based on clinical signs, such as leg deformity and inability to move the limb. Initial treatment focuses on closed reduction to realign the hip, ideally performed as soon as possible to prevent complications like avascular necrosis. Follow-up care, including immobilization and physical therapy, may be constrained, increasing the risk of long-term disability if not adequately managed.
A 7-year-old boy presents to the emergency department after a fall from a swing, with severe left hip pain and inability to move his leg. Examination reveals a shortened, flexed, adducted, and internally rotated left leg. X-rays confirm a posterior hip dislocation. The hip is successfully reduced under sedation, and follow-up X-rays show proper alignment. The boy is referred to an orthopedic surgeon for further evaluation and rehabilitation to ensure proper healing and prevent complications.
Related Topics
1. Brian Weatherford, Hip Dislocation, May 2 2024. Orthobullets. Available at: https://www.orthobullets.com/trauma/1035/hip-dislocation
2. Dawson-Amoah, Kwesi & Raszewski, Jesse & Duplantier, Neil & Waddell, Bradford. (2018). Dislocation of the Hip: A Review of Types, Causes, and Treatment. Ochsner Journal. 18. 242-252. 10.31486/toj.17.0079.
3. Waddell BS, Mohamed S, Glomset JT, Meyer MS. A Detailed Review of Hip Reduction Maneuvers: A Focus on Physician Safety and Introduction of the Waddell Technique. Orthop Rev (Pavia). 2016 Mar 21;8(1):6253. doi: 10.4081/or.2016.6253. PMID: 27114811; PMCID: PMC4821229.
4. Travis E. Clegg, Craig S. Roberts, Joseph W. Greene, Brad A. Prather, Hip dislocations—Epidemiology, treatment, and outcomes, Injury, Volume 41, Issue 4, 2010, Pages 329-334, ISSN 0020-1383, https://doi.org/10.1016/j.injury.2009.08.007. (https://www.sciencedirect.com/science/article/pii/S0020138309004392)
5. CMC Compedium. Posterior Hip Dislocation December 2nd 2016. Available at: https://www.cmcedmasters.com/ortho-blog/posterior-hip-dislocation Accessed January 21st 2025.
6. Hogan, Teresita. (2004). Hip joint dislocation reduction. Emergency medicine procedures. 632-639.
7.@inproceedings{Murray2013Table5S, title={Table 56-1 Structures within Compartments of the Thigh},author={Brittany L. Murray}, year={2013}, url={https://api.semanticscholar.org/CorpusID:3843892}}
8. Kwesi Dawson-Amoah, Jesse Raszewski, Neil Duplantier and Bradford Sutton Waddell Dislocation of the hip’: A Review of Types, Causes, and Treatment. Ochsner Journal September 2018, 18 (3) 242-252; DOI: https://doi.org/10.31486/toj.
17.0079

More topics to explore
Author's details
Reviewer's details
Hip Dislocation
- Background
- Symptoms
- Clinical findings
- Differential diagnosis
- Investigations
- Treatment
- Follow-up
- Prevention and control
- Further readings
The hip joint is a ball and socket type of synovial joint. Dislocation is an orthopaedic emergency as immediate reduction is needed to prevent destruction of the joint. Hip dislocation needs a high amount of energy to occur. Diagnosis can be confirmed with pelvic radiograph. Treatment involves emergency reduction of the dislocation, check stability after reduction and do a control radiograph to confirm reduction and rule out other any associated fracture. Hip dislocation can affect both native and artificial joints (total hip replacement).
Hip dislocation is the second most common dislocation after shoulder in the major joints.
1. Brian Weatherford, Hip Dislocation, May 2 2024. Orthobullets. Available at: https://www.orthobullets.com/trauma/1035/hip-dislocation
2. Dawson-Amoah, Kwesi & Raszewski, Jesse & Duplantier, Neil & Waddell, Bradford. (2018). Dislocation of the Hip: A Review of Types, Causes, and Treatment. Ochsner Journal. 18. 242-252. 10.31486/toj.17.0079.
3. Waddell BS, Mohamed S, Glomset JT, Meyer MS. A Detailed Review of Hip Reduction Maneuvers: A Focus on Physician Safety and Introduction of the Waddell Technique. Orthop Rev (Pavia). 2016 Mar 21;8(1):6253. doi: 10.4081/or.2016.6253. PMID: 27114811; PMCID: PMC4821229.
4. Travis E. Clegg, Craig S. Roberts, Joseph W. Greene, Brad A. Prather, Hip dislocations—Epidemiology, treatment, and outcomes, Injury, Volume 41, Issue 4, 2010, Pages 329-334, ISSN 0020-1383, https://doi.org/10.1016/j.injury.2009.08.007. (https://www.sciencedirect.com/science/article/pii/S0020138309004392)
5. CMC Compedium. Posterior Hip Dislocation December 2nd 2016. Available at: https://www.cmcedmasters.com/ortho-blog/posterior-hip-dislocation Accessed January 21st 2025.
6. Hogan, Teresita. (2004). Hip joint dislocation reduction. Emergency medicine procedures. 632-639.
7.@inproceedings{Murray2013Table5S, title={Table 56-1 Structures within Compartments of the Thigh},author={Brittany L. Murray}, year={2013}, url={https://api.semanticscholar.org/CorpusID:3843892}}
8. Kwesi Dawson-Amoah, Jesse Raszewski, Neil Duplantier and Bradford Sutton Waddell Dislocation of the hip’: A Review of Types, Causes, and Treatment. Ochsner Journal September 2018, 18 (3) 242-252; DOI: https://doi.org/10.31486/toj.
17.0079

Content
Author's details
Reviewer's details
Hip Dislocation
Background
The hip joint is a ball and socket type of synovial joint. Dislocation is an orthopaedic emergency as immediate reduction is needed to prevent destruction of the joint. Hip dislocation needs a high amount of energy to occur. Diagnosis can be confirmed with pelvic radiograph. Treatment involves emergency reduction of the dislocation, check stability after reduction and do a control radiograph to confirm reduction and rule out other any associated fracture. Hip dislocation can affect both native and artificial joints (total hip replacement).
Hip dislocation is the second most common dislocation after shoulder in the major joints.
Further readings
1. Brian Weatherford, Hip Dislocation, May 2 2024. Orthobullets. Available at: https://www.orthobullets.com/trauma/1035/hip-dislocation
2. Dawson-Amoah, Kwesi & Raszewski, Jesse & Duplantier, Neil & Waddell, Bradford. (2018). Dislocation of the Hip: A Review of Types, Causes, and Treatment. Ochsner Journal. 18. 242-252. 10.31486/toj.17.0079.
3. Waddell BS, Mohamed S, Glomset JT, Meyer MS. A Detailed Review of Hip Reduction Maneuvers: A Focus on Physician Safety and Introduction of the Waddell Technique. Orthop Rev (Pavia). 2016 Mar 21;8(1):6253. doi: 10.4081/or.2016.6253. PMID: 27114811; PMCID: PMC4821229.
4. Travis E. Clegg, Craig S. Roberts, Joseph W. Greene, Brad A. Prather, Hip dislocations—Epidemiology, treatment, and outcomes, Injury, Volume 41, Issue 4, 2010, Pages 329-334, ISSN 0020-1383, https://doi.org/10.1016/j.injury.2009.08.007. (https://www.sciencedirect.com/science/article/pii/S0020138309004392)
5. CMC Compedium. Posterior Hip Dislocation December 2nd 2016. Available at: https://www.cmcedmasters.com/ortho-blog/posterior-hip-dislocation Accessed January 21st 2025.
6. Hogan, Teresita. (2004). Hip joint dislocation reduction. Emergency medicine procedures. 632-639.
7.@inproceedings{Murray2013Table5S, title={Table 56-1 Structures within Compartments of the Thigh},author={Brittany L. Murray}, year={2013}, url={https://api.semanticscholar.org/CorpusID:3843892}}
8. Kwesi Dawson-Amoah, Jesse Raszewski, Neil Duplantier and Bradford Sutton Waddell Dislocation of the hip’: A Review of Types, Causes, and Treatment. Ochsner Journal September 2018, 18 (3) 242-252; DOI: https://doi.org/10.31486/toj.
17.0079
Advertisement

