Author's details
- Dr. Khashau Eleburuike.
- MBBS (Ilorin) MSc. Global Health Karolinska Institute.
- Resident doctor in family medicine in Northen Sweden.
Reviewer's details
- Dr. Habibat Suberu.
- MBBS; FMCPaed
- Date Uploaded: 2024-10-13
- Date Updated: 2025-02-03
Diarrhoeal Diseases in children less than 5 years old
Summary
Diarrheal disease is a leading cause of morbidity and mortality world-wide especially in low-income countries due to underlying malnutrition especially among children less than 5 years old. Diarrhoea is defined as increased frequency and fluidity of stool passed- usually more than 3 stool episodes in 24 hours. It is caused by by different infectious or inflammatory processes in the intestine affecting the secretory and absorptive capacity of the intestine. It can be clinically classified as acute watery diarrhoea; acute bloody diarrhoea or dysentery; prolonged diarrhoea lasting 7 to 14 days; persistent diarrhoea lasting 14 days or longer. The mechanism of diarrhoea includes- secretory; osmotic; increased intestinal motility and mucosal invasion.
In the acute phase, dehydration is a major cause of death while after 2 weeks, malnutrition, non-intestinal infection worsens the outcome. Destruction of the intestinal mucosa occurs with acute dysentery.
Most diarrheal illness is due to infections which could be viral, bacterial, or parasitic infections. There are also non-infectious causes of childhood diarrhoea.
Acute watery diarrhoea in children less than 2 years is mostly caused by Rotavirus. In other age groups, the etiological agents of watery diarrhoea are Enterotoxigenic Escherichia coli (ETEC) which is common in older children and adults; Vibrio cholera O1 and O139 whereby the stool is like “rice-water" come as endemics or epidemics. Cryptosporidium is common in infants or HIV infected children. Noroviruses present with a sudden onset of vomiting and diarrhoea.
- Acute bloody diarrhoea or dysentery is often caused by Shigella spp that comes with epidemics and patients have severe disease with complications like sepsis, intestinal perforations, megacolon, rectal prolapse seizures and encephalopathy.
- Enteroinvasive Escherichia coli (EIEC) present with similar symptoms as Shigella.
- Enterohemorrhagic Escherichia coli (EHEC) is like Shigella, and patients have increased risk of developing haemolytic uremic syndrome.
- Nontyphoidal Salmonella enterica infection is common among infants, elderly and immunocompromised children. Campylobacter jejuni infection presents with diarrhoea in young children and acute mesenteric lymphadenitis in older children mimicking appendicitis. It could also lead to Guillain-Barré syndrome.
- Entamoeba histolytica a protozoon that is similar in presentation to Shigella and in rare cases lead till hepatic abscess
- Adenoviruses cause both watery diarrhoea and dysentery.
Non infectious causes of diarrhoea in children includes:
- Carbohydrate malabsorption (congenital or acquired)
- Functional diarrhea, eg, diarrhea-predominant irritable bowel syndrome, “chronic nonspecific diarrhea”
- Inflammatory bowel disease
- Pancreatic insufficiency
- Immunodeficiency syndromes
- Motility disorders
- Neuroendocrine tumours
- Hyperthyroidism
- Congenital diarrhoea
- Drug-related
Frequent stools more than 3 times daily or that which differs from the norm because breastfed children could have more stool. It can be watery or with blood.
- Acute diarrhoea occurs within hours to days.
- Persistent diarrhoea is more than 2 weeks
- Severe malnutrition like kwashiorkor and marasmus with diarrhoea present even with severe systemic dehydration, vitamin deficiency and heart failure.
An important consideration in the management of a child with diarrhoea is the accurate assessment for dehydration. The degree of dehydration determines the urgency of the situation and the volume of fluid required for rehydration.
In the early stage of dehydration the child usually has no symptoms.
At the intermediate stage of dehydration: patient could be restless, thirsty or irritable. May have sunken eyes and fontanelle or decreased skin turgor when the abdomen is gently pinched, and it takes > 2 seconds to go back to its original level.
When the dehydration becomes severe, patients manifest with hypovolemic shock. There is reduced urine production, unconsciousness, cool clammy extremities, undetectable radial pulse and hypotonia.
Malaria: history of mosquito bite, fever. Bacterial meningitis: diarrhoea with fever and seizures Sepsis. Appendicitis. Intussusception. Hyperthyroidism. HIV. Neoplastic diseases. Milk intolerance is rare but should be suspected if stool increases as milk is given.
- Initial evaluation includes electrolytes, BUN and creatinine. Electrolytes like sodium could be high when patient is given sweetened food or too concentrated formulas or fluid with too much salt. Hyponatremia (Sodium <130 mmol/l) if the child is given plain water or low salt. Hypokalaemia (Potassium <3mmol/l) occurs when the loss of potassium is not replaced during diarrhoea.
- Stool specimen should be examined for mucus, blood, leucocytes and parasitic agents.
- Faecal culture is recommended for patients with fever, profuse diarrhoea and dehydration or if HUS is suspected.
- Full blood count
In children with mild to moderate dehydration it is important to give Oral rehydration therapy. Salted drinks like yoghurt, chicken soup, rice water can be given to children at home. Avoid sweetened drinks, carbonated drinks as it may lead to osmotic diarrhoea or hypernatremia. Coffee and medicinal teas should not be given because of their diuretic or purgative effects.
Weigh the child without clothes. There should be no delay in treatment of dehydration even if there is no weighing scale because an estimate of weight can be done using weight for the child’s age. A child with no dehydration an estimate of <5% of body weight and a fluid deficit of <50 ml/kg can be given. In moderate dehydration, 5-10% of body weight and an estimate of 50-100ml/kg. With severe dehydration a fluid deficit of >10% give a fluid of >100ml/kg. A child showing sign of overhydration such as puffy eyes should not be given ORS nor diuretics but breastmilk.
Patients with severe dehydration start with intravenous fluids but give oral rehydration when stable. In severe dehydration 100 ml/kg Ringer Lactate whereby the first 30ml/kg is given within the first 1 hour for infants and 30 minutes for older children. The remaining 70 ml/kg should be given in 5 hours for infants and 2½ hours for older children.
An average of 75 ml/kg Ringer’s Lactate in 4 hours if a child with moderate dehydration persists in diarrhoea and have vomiting. In settings without intravenous fluid give ORS via a nasogastric tube 20 ml/kg/hour. If a child vomits or the abdomen distends give slowly and evaluate hourly
High nutritious foods given during and after diarrhoea reduce the risk of complications. It is important to give small amounts of staple food available in the environment as frequently as every 3-4 hours for infants and 1-2 hours in older children. Assessment of the patient every 15-30 minutes.
Zinc: Giving 10-20mg Zinc within the duration of diarrhoea or 10-14 days improve recovery of the intestinal mucosa and immune system. It could be given as a supplement
Antibiotics and antidiarrheal agents should not be routinely used. Antimicrobial could be given in suspected Cholera or Shigella (Ciprofloxacin). Loperamide can lead to abdominal distension. and paralytic ileus.
Antimicrobials that are ineffective for treatment of Shigellosis
- metronidazole • streptomycin · • tetracyclines · • chloramphenicol · • sulfonamides • amoxycillin • nitrofurans (e.g. nitrofurantoin, furazolidone) • aminoglycosides (e.g. gentamicin, kanamycin) • first and second generation cephalosporins (e.g. cephalexin, cefamandole Click here to enter text.
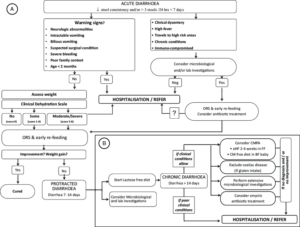
TREATMENT ALGORITHM FOR ACUTE INFECTIOUS DIARRHOEA.
Children with signs of dehydration should be followed up after 2 days and if not better referred to the hospital.
Parents should be educated about red flags in diarrhoea that should make them seek medical care immediately.
Breastfeeding
Sanitation: hand washing
Use of clean water
Food safety: Washing of hands before cooking. Heat food before eating. Proper cooking of food
Appropriate disposal of faeces
Immunization against rota virus infection.
Lactobacillus acidophilus – a probiotic- reduces the incidence of community acquired and antibiotic associated diarrhoea in children treated with oral antibiotics for other infectious diseases.
Diarrheal diseases remain a leading cause of morbidity and mortality in children under 5 years in sub-Saharan Africa, primarily due to poor sanitation, inadequate access to clean water, and malnutrition. Effective prevention through improved hygiene, safe drinking water, vaccination (such as rotavirus), and prompt treatment with oral rehydration solutions and zinc can significantly reduce the disease burden and save lives in this vulnerable population.
Mrs K brings her 18-month-old son to the primary health centre presenting with loose stool 4 times daily in a week. First, he could eat as usual and drink but within the past 2 days his appetite diminished. The stool is watery, slimy with no blood. He stays in a daycare and other children have similar symptoms. He had 2 episodes of vomiting yesterday. Before the start of symptoms, he ate pap prepared by his mom.
On examination a healthy boy, a bit tired, sunken eyes, minimal tears when he cried. Normal radial pulse palpated, normal skin turgor. Body weight 10 kg
A working diagnosis of diarrhoea was made probably due to Rotavirus due to his age. Mother was instructed to give ORS as frequently as possible especially after diarrhoea or vomiting. 50ml/kg per day. Education of the mother about proper food handling, hand hygiene, clean water or boiling of water. He should also be fed small quantities 3-4 hours per day. A follow-up visits to the health-centre after 2 days.
After 2 days of conservative management, Mrs K says that her son had worsened with more frequent stool that is watery, refused ORT, vomits, tired and lost weight. His mom became desperate and gave him juice and soft drinks which he takes. While examining the patient he is lethargic, dry lips, sunken eyes, His radial pulse is feeble, he has cold damp hands. A clinical judgement of severe dehydration was made. An attempt to find a line for intravenous Ringer lactate was futile. A nasogastric tube (NG) was passed, he got 200 ml per hour, but he started vomiting and removed the NG tube. A new attempt was made for the intravenous line that was successful. He got 100 ml/kg of Ringer lactate; the first 300 ml was given within the first hour. He became better and oral nutrition was reintroduced.
Before discharge home, Mrs K was educated about appropriate diet during diarrhoea, importance of per oral nutrition when a child has diarrhoea, hygiene and proper disposal of faeces.
- The treatment of diarrhoea. A manual for physicians and other senior health workers. 4th rev. World Health Organization 2005. ISBN 92 4 159318 0 (NLM classification: WS 312) https://iris.who.int/bitstream/handle/10665/43209/9241593180.pdf?sequence=1
- Preventing Diarrhoea Through Better Water, Sanitation and Hygiene. Exposures and impacts in low- and middle-income countries. © World Health Organization 2014. ISBN 978 92 4 156482 3 (NLM classication: WA 675) https://iris.who.int/bitstream/handle/10665/150112/9789241564823_eng.pdf?sequence=1
- Therapeutic Value of Zinc Supplementation in Acute and Persistent Diarrhea: A Systematic ReviewArchana Patel, Manju Mamtani,,Michael J. Dibley, Neetu Badhoniya, Hemant Kulkarni Published: April 28, 2010 https://doi.org/10.1371/journal.pone.0010386
- World Health Organization. (2002). Reduced osmolarity : oral rehydration salts (ORS) formulation : a report from a meeting of experts jointly organised by UNICEF and WHO : UNICEF house, New York, USA, 18 July 2001. World Health Organization. https://iris.who.int/handle/10665/67322
- Omona, S., Malinga, G.M., Opoke, R. et al.Prevalence of diarrhoea and associated risk factors among children under five years old in Pader District, northern Uganda. BMC Infect Dis 20, 37 (2020). https://doi.org/10.1186/s12879-020-4770-0
- Demissie GD, Yeshaw Y, Aleminew W, Akalu Y. Diarrhea and associated factors among under five children in sub-Saharan Africa: Evidence from demographic and health surveys of 34 sub-Saharan countries. PLoS One. 2021 Sep 20;16(9):e0257522. doi: 10.1371/journal.pone.0257522. PMID: 34543347; PMCID: PMC8452002.
- Guarino, Alfredo & Aguilar, Juliet & Berkley, James & Broekaert, Ilse & Vázquez, Rodrigo & Holtz, Lori & Vecchio, Andrea & Meskini, Toufik & Moore, Sean & Rivera Medina, Juan Francisco & Sandhu, Bhupinder & Smarrazzo, Andrea & Szajewska, Hania & Treepongkaruna, Suporn. (2020). Acute Gastroenteritis in Children of the World: What Needs to Be Done?. Journal of Pediatric Gastroenterology and Nutrition. 70. 1. 10.1097/MPG.0000000000002669.
- Nelson essentials of Pediatrics 8th edition; chapter 113; pg 410-413

Author's details
Reviewer's details
Diarrhoeal Diseases in children less than 5 years old
- Background
- Symptoms
- Clinical findings
- Differential diagnosis
- Investigations
- Treatment
- Follow-up
- Prevention and control
- Further readings
Diarrheal disease is a leading cause of morbidity and mortality world-wide especially in low-income countries due to underlying malnutrition especially among children less than 5 years old. Diarrhoea is defined as increased frequency and fluidity of stool passed- usually more than 3 stool episodes in 24 hours. It is caused by by different infectious or inflammatory processes in the intestine affecting the secretory and absorptive capacity of the intestine. It can be clinically classified as acute watery diarrhoea; acute bloody diarrhoea or dysentery; prolonged diarrhoea lasting 7 to 14 days; persistent diarrhoea lasting 14 days or longer. The mechanism of diarrhoea includes- secretory; osmotic; increased intestinal motility and mucosal invasion.
In the acute phase, dehydration is a major cause of death while after 2 weeks, malnutrition, non-intestinal infection worsens the outcome. Destruction of the intestinal mucosa occurs with acute dysentery.
- The treatment of diarrhoea. A manual for physicians and other senior health workers. 4th rev. World Health Organization 2005. ISBN 92 4 159318 0 (NLM classification: WS 312) https://iris.who.int/bitstream/handle/10665/43209/9241593180.pdf?sequence=1
- Preventing Diarrhoea Through Better Water, Sanitation and Hygiene. Exposures and impacts in low- and middle-income countries. © World Health Organization 2014. ISBN 978 92 4 156482 3 (NLM classication: WA 675) https://iris.who.int/bitstream/handle/10665/150112/9789241564823_eng.pdf?sequence=1
- Therapeutic Value of Zinc Supplementation in Acute and Persistent Diarrhea: A Systematic ReviewArchana Patel, Manju Mamtani,,Michael J. Dibley, Neetu Badhoniya, Hemant Kulkarni Published: April 28, 2010 https://doi.org/10.1371/journal.pone.0010386
- World Health Organization. (2002). Reduced osmolarity : oral rehydration salts (ORS) formulation : a report from a meeting of experts jointly organised by UNICEF and WHO : UNICEF house, New York, USA, 18 July 2001. World Health Organization. https://iris.who.int/handle/10665/67322
- Omona, S., Malinga, G.M., Opoke, R. et al.Prevalence of diarrhoea and associated risk factors among children under five years old in Pader District, northern Uganda. BMC Infect Dis 20, 37 (2020). https://doi.org/10.1186/s12879-020-4770-0
- Demissie GD, Yeshaw Y, Aleminew W, Akalu Y. Diarrhea and associated factors among under five children in sub-Saharan Africa: Evidence from demographic and health surveys of 34 sub-Saharan countries. PLoS One. 2021 Sep 20;16(9):e0257522. doi: 10.1371/journal.pone.0257522. PMID: 34543347; PMCID: PMC8452002.
- Guarino, Alfredo & Aguilar, Juliet & Berkley, James & Broekaert, Ilse & Vázquez, Rodrigo & Holtz, Lori & Vecchio, Andrea & Meskini, Toufik & Moore, Sean & Rivera Medina, Juan Francisco & Sandhu, Bhupinder & Smarrazzo, Andrea & Szajewska, Hania & Treepongkaruna, Suporn. (2020). Acute Gastroenteritis in Children of the World: What Needs to Be Done?. Journal of Pediatric Gastroenterology and Nutrition. 70. 1. 10.1097/MPG.0000000000002669.
- Nelson essentials of Pediatrics 8th edition; chapter 113; pg 410-413

Content
Author's details
Reviewer's details
Diarrhoeal Diseases in children less than 5 years old
Background
Diarrheal disease is a leading cause of morbidity and mortality world-wide especially in low-income countries due to underlying malnutrition especially among children less than 5 years old. Diarrhoea is defined as increased frequency and fluidity of stool passed- usually more than 3 stool episodes in 24 hours. It is caused by by different infectious or inflammatory processes in the intestine affecting the secretory and absorptive capacity of the intestine. It can be clinically classified as acute watery diarrhoea; acute bloody diarrhoea or dysentery; prolonged diarrhoea lasting 7 to 14 days; persistent diarrhoea lasting 14 days or longer. The mechanism of diarrhoea includes- secretory; osmotic; increased intestinal motility and mucosal invasion.
In the acute phase, dehydration is a major cause of death while after 2 weeks, malnutrition, non-intestinal infection worsens the outcome. Destruction of the intestinal mucosa occurs with acute dysentery.
Further readings
- The treatment of diarrhoea. A manual for physicians and other senior health workers. 4th rev. World Health Organization 2005. ISBN 92 4 159318 0 (NLM classification: WS 312) https://iris.who.int/bitstream/handle/10665/43209/9241593180.pdf?sequence=1
- Preventing Diarrhoea Through Better Water, Sanitation and Hygiene. Exposures and impacts in low- and middle-income countries. © World Health Organization 2014. ISBN 978 92 4 156482 3 (NLM classication: WA 675) https://iris.who.int/bitstream/handle/10665/150112/9789241564823_eng.pdf?sequence=1
- Therapeutic Value of Zinc Supplementation in Acute and Persistent Diarrhea: A Systematic ReviewArchana Patel, Manju Mamtani,,Michael J. Dibley, Neetu Badhoniya, Hemant Kulkarni Published: April 28, 2010 https://doi.org/10.1371/journal.pone.0010386
- World Health Organization. (2002). Reduced osmolarity : oral rehydration salts (ORS) formulation : a report from a meeting of experts jointly organised by UNICEF and WHO : UNICEF house, New York, USA, 18 July 2001. World Health Organization. https://iris.who.int/handle/10665/67322
- Omona, S., Malinga, G.M., Opoke, R. et al.Prevalence of diarrhoea and associated risk factors among children under five years old in Pader District, northern Uganda. BMC Infect Dis 20, 37 (2020). https://doi.org/10.1186/s12879-020-4770-0
- Demissie GD, Yeshaw Y, Aleminew W, Akalu Y. Diarrhea and associated factors among under five children in sub-Saharan Africa: Evidence from demographic and health surveys of 34 sub-Saharan countries. PLoS One. 2021 Sep 20;16(9):e0257522. doi: 10.1371/journal.pone.0257522. PMID: 34543347; PMCID: PMC8452002.
- Guarino, Alfredo & Aguilar, Juliet & Berkley, James & Broekaert, Ilse & Vázquez, Rodrigo & Holtz, Lori & Vecchio, Andrea & Meskini, Toufik & Moore, Sean & Rivera Medina, Juan Francisco & Sandhu, Bhupinder & Smarrazzo, Andrea & Szajewska, Hania & Treepongkaruna, Suporn. (2020). Acute Gastroenteritis in Children of the World: What Needs to Be Done?. Journal of Pediatric Gastroenterology and Nutrition. 70. 1. 10.1097/MPG.0000000000002669.
- Nelson essentials of Pediatrics 8th edition; chapter 113; pg 410-413
Advertisement

