Author's details
- Dr ABUBAKAR MUSA MOHAMMED
- (MBBS, FWACS)
- CONSULTANT NEUROSURGEON. FEDERAL UNIVERSITY TEACHING HOSPITAL, DUTSE, NIGERIA. dwinfos@yahoo.co.uk,
Reviewer's details
- Dr Ajiboye lukman Olalekan
- (MBBS, FMCOrtho, FWACS, FICS, FACS FAOSpine).
- Associate Professor, Consultant Orthopedic, Spine and Trauma Surgeon, Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria
- Date Uploaded: 2024-10-16
- Date Updated: 2025-12-20
General Overview of Low Back Pain, LBP (AKA, LUMBAGO)
Key Messages
- Low back pain (LBP) is a common global health issue, affecting up to 80% of adults and leading to disability and missed workdays.
- Causes include mechanical strain, trauma, age-related degeneration, infections, tumors, and arthritis; correct diagnosis is crucial for effective treatment.
- Symptoms range from localized pain to radiating limb pain, numbness, weakness, and in severe cases, paralysis or bladder/bowel dysfunction.
- Management spans conservative care (rest, physiotherapy, medications) to surgery for severe or unresponsive cases.
Low back pain (LBP) or Lumbago, denotes the presence of painful sensation in the lower back in varying degrees of severity and duration, which can radiate down one or both lower limbs, and may be complicated by limbs weakness, bowel and bladder voiding difficulties as well as erectile dysfunction in males. The management of LBP varies from simple physical exercises to complex low back surgeries, and the ultimate cure depends to a greater extent on the cause of the pain. Understanding the root causes of LBP and recognizing it’s red-flag symptoms, can help in early diagnosis and effective management, as well as averting some of the complications mentioned above.
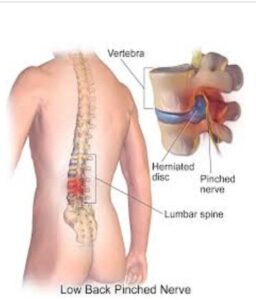
Courtesy: Physio-pedia.com/Disc_Herniation.
LBP is a common ailment that affects millions of people worldwide. It is a global health concern, ranking as one of the leading causes of disability, missed workdays and a reason for specialist doctor visits. in Nigeria, the prevalence is estimated to be between 33-73%.
People of all ages and backgrounds can suffer from LBP, however, obese individuals and cigarette smokers have higher preponderance. However, the incidence is higher after age of 45, especially among women, wight lifter and people low activities (sedentary lifestyles). Studies have indicated that nearly 80% of all adults will experience low back pain at some point in their lives.
LBP can arise from various factors; the most common ones include the following: -
- Mechanical factors =
- Sudden or persistent poor posture which bends the backbone (spine) and cause excessive strain on the back muscles, ligaments and inter-vertebral Examples include lifting a heavy weight from an abnormal stooping posture, reclining on a sofa while watching a TV programme for several hours, prolonged sitting or standing while at work, usage of extra-soft beddings that tends to bend the spine, etc.)
- Traumatic spine injuries and related inter-vertebral disc herniation, spine fracture or dislocation (spondylolisthesis)
- Age-related degeneration of the spine (spondylosis)
- Spine infections, especially Tuberculosis (AKA Pott's disease)
- Tumors of the bony spine (vertebral column), or of the spinal cord and nerves
- Arthritis of the inter-vertebral (facet) joints
The LBP commences when sensory nerves in the area are involved by any of the conditions listed above, either indirectly by nerve irritation or directly by nerve compression, and even nerve damage from disease infiltration. Since the nerves run along the entire length of the lower limbs, the same pain can be felt to be radiating down the affected limb(s).
By extension, when the motor nerves are similarly affected there will be associated varying degrees of limbs weakness which potentially can end in complete paralysis, as well as sphincteric dysfunctions which can lead to faecal and/or urinary voiding difficulties. In males, there may also be erectile dysfunction which can cause impotency. These latter symptoms signify an emergency condition called cauda equina syndrome that requires immediate intervention to prevent permanent irreversible nerves injury.
Due to the varied nature of LBP causes, correct diagnosis of a specific cause in each patient is very crucial for tailored treatment and possible cure.
As mentioned above, some of the common presenting symptoms and signs of LBP include the following: -
- Presence of persistent ache, pain or discomfort in the lower back, the intensity and duration of which can vary.
- Pain that radiates along one or both lower limbs (AKA sciatica) especially during prolonged standing, sitting or walking (Neurogenic claudication). Sometimes, affected individuals will have to pause and rest before resuming walking or other
- Reduced or loss of sensations in the affected areas
- Muscle spasms and stiffness after a pronged disuse of joint in the lower back and the
- Limited mobility of lower limbs joints
- Paralysis or lower limb paralysis
- Bowel and/or bladder dysfunctions, causing faecal and/or urine retention (inability to void), or incontinence (involuntary voiding).
- Erectile dysfunction (impotence) in Males
The Visual Analog Scale (VAS) is a commonly employed tool used by clinicians to assess the degree of pain from 0-10 (i.e no pain-worst pain, respectively) as rated by each patient objectively. This rating will give an insight about the pre-and post- treatment pain status of the patient, thus, determining the efficacy of the treatment.
Since accurate diagnosis of LBP is essential for appropriate treatment or cure, spine specialists often recommend various investigations including the following: -
- Plain Radiograph (X-ray): - To visualize the bony spine (vertebral column) and rule out fractures, degenerative changes, bony destructions or tumor deposits.
- MRI (Magnetic Resonance Imaging): - To get detailed images of soft tissues like herniated discs and compressed nerve roots, as well as spinal cord compression or other lesions like swelling (oedema/myelopathy), transection, tumors and fluid collections (hematoma, pus/abscesses, syrinx).
- CT (Computed Tomography) Scans: - Sometimes used for further evaluation of bone and soft tissues.
- Blood Tests: - To check for underlying causative conditions like infections, inflammatory disorders or metastatic cancers (especially from paired organs, like lungs, breasts, kidneys and prostate).
- Baseline medical checks may also be undertaken if there’s prospect of surgical intervention, most especially in elderly patients having other medical co-
Treating LBP involves a multidisciplinary approach tailored to an individual patient's needs based primarily on a diagnosis, severity of condition and presence of other medical co-morbidities. The following measures are usually observed in ascending order: -
- Conservative Management: - Most cases of low back pain can be managed conservatively with adequate bed rest, targeted physiotherapy, posture/back education and pain-relief Exercises to strengthen core muscles and improve posture can be highly effective.
- Pain relievers (analgesics): Non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and in some cases, prescription narcotics may be used. It is noteworthy that dyspeptic individuals on NSAIDs may experience worsening symptoms of dyspepsia and gastro-intestinal bleeds, therefore, anti-ulcer drugs should be added for them, or alternative analgesics should be
- Steroid Injections: - Transforaminal and epidural steroid injections for specific nerve blockage can offer temporary relief from mild to moderate low back Sometimes, utilizing Methylprednisolone mixed with plain Lidocaine and Bupivacaine can offer long-term (or even permanent) relief of symptoms in certain individuals.
- Surgery: - this is typically reserved for cases where the conservative treatments fail or when there is an identifiable structural lesion causing severe nerve roots compression (foraminal or extra-foraminal stenosis) and spinal cord or cauda equina compression (canal stenosis). Example of such lesions include a large herniated inter-vertebral disc, vertebral fracture or collapse, high grade vertebral dislocation (spondylolisthesis), spinal abscess collection or an operable spinal
- Chemo-radiation and other specific systemic drug therapies may exclusively be considered in metastatic malignancies, with or without the surgical
Both out- and in-patients being managed for LBP will be followed-up closely to monitor and record the progress being achieved. It is highly worthy of note that LBP due to disc hernia can recur even after most sophisticated surgical intervention, either as new disc prolapses (adjacent disc disease) or from the previously treated disc space (disc re-herniation). All patients need to understand these phenomena right from their first visit in the spine clinic.
The prognosis of LBP depends on various factors including the age of patients, the causative agent of factor, the duration or severity of the condition, the associated complication arising from the disease, as well as the presence of other medical co- morbidities. As a typical example, a young healthy individual with an acute single level disc hernia arising from heavy weightlifting will have an excellent prognosis and much better treatment outcome compared to an elderly hypertensive person with metastatic tumor to the spine.
Remember that prevention is often the best treatment. Below are some healthy tips to help minimize the risk of developing (or progression of) LBP: -
- Maintaining a healthy One of the best ways to do this is by reducing dietary intake (especially carbohydrate or sugary foods) and observing regular fasting like twice weekly.
- Regular Isotonic exercises, example jogging, riding a bicycle or walking on the treadmill
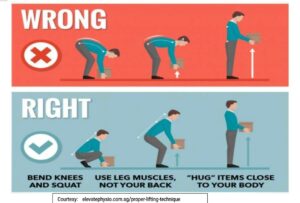
- Back education to practice good postures (see the inserted pics): -
- Sitting down with the back in erect position supported against the seatback or wall
- Sleeping on flat surfaces, but not necessarily on the hard floor!
- Strapping school backpacks squarely on both shoulders and placing on the
- Avoiding lifting heavy objects altogether, but, if necessary, try and lift the weight keeping the back erect and straight while flexing the knees, not bending the back and flexing the hips.



LBP is a common condition affecting individuals of all ages worldwide, with mechanical factors being the most common documented causes. Since it is of great importance to ensure correct diagnosis of LBP, it is essential to seek professional medical advice early to institute proper evaluation and personalized care, as well as to prevent potentially disastrous outcomes like permanent nerve injury.
DO, a 45-year-old farmer from Eastern Nigeria, presented with a 6-month history of persistent low back pain that worsened over time, radiating to his left leg with occasional numbness. The pain was aggravated by his heavy manual labor and was not relieved by over-the-counter painkillers.
Physical examination revealed tenderness in the lower lumbar spine, a positive straight leg raise test on the left, and mild sensory changes in the left foot. X-rays showed degenerative changes at L4-L5, indicating possible lumbar disc herniation and degenerative disc disease.
DO was treated with NSAIDs, muscle relaxants, and physical therapy, along with advice on modifying his work habits. His symptoms improved over several weeks, and further imaging was not required. He continues to manage his condition with exercises and lifestyle adjustments.
Related Topics
- Airenakho E, Cyril OE, Blessyn OA, et Epidemiology of LBP: frequency, risk factors and patterns in South-South Nigeria. Reumatologia 2023;61(5):360-367, doi:https://doi.org/10.5114/reum/173377
- Bello B, Bello A systematic review on the prevalence of LBP in Nigeria. MiddleEast J Rahabil Health 2017;4:e45262, doi:10.5812/mejrh.45262
- Kahere M, Ginindza A cross-sectional hospital-based study of correlates of disability in patients with chronic LBP in Kwazulu-Natal, South Africa. BMC Musculoskeletal Disord 2022;23:438, doi:10.1186/s12891-022-05397-4.
- Nicol V, Verdaguer C, Daste C, et Chronic LBP: a narrative review of recent international guidelines for diagnosis and conservative treatment. J Clin Med 2023;12:1685, doi:10.3390/jcm12041685
- Chen S, Chen M, Wu X, et al. Global, regional and national burden of LBP 1990-2019: a systematic analysis of the Global Burden of Disease study 2019. J Orthop Transl 2022; 32:49-58, doi:10.1016/j.jot.2021.07.005

More topics to explore
Author's details
Reviewer's details
General Overview of Low Back Pain, LBP (AKA, LUMBAGO)
- Background
- Symptoms
- Clinical findings
- Differential diagnosis
- Investigations
- Treatment
- Follow-up
- Prevention and control
- Further readings
Low back pain (LBP) or Lumbago, denotes the presence of painful sensation in the lower back in varying degrees of severity and duration, which can radiate down one or both lower limbs, and may be complicated by limbs weakness, bowel and bladder voiding difficulties as well as erectile dysfunction in males. The management of LBP varies from simple physical exercises to complex low back surgeries, and the ultimate cure depends to a greater extent on the cause of the pain. Understanding the root causes of LBP and recognizing it’s red-flag symptoms, can help in early diagnosis and effective management, as well as averting some of the complications mentioned above.
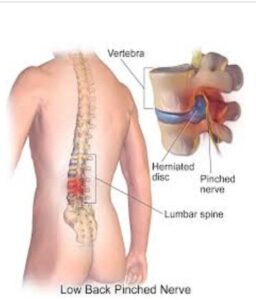
Courtesy: Physio-pedia.com/Disc_Herniation.
- Airenakho E, Cyril OE, Blessyn OA, et Epidemiology of LBP: frequency, risk factors and patterns in South-South Nigeria. Reumatologia 2023;61(5):360-367, doi:https://doi.org/10.5114/reum/173377
- Bello B, Bello A systematic review on the prevalence of LBP in Nigeria. MiddleEast J Rahabil Health 2017;4:e45262, doi:10.5812/mejrh.45262
- Kahere M, Ginindza A cross-sectional hospital-based study of correlates of disability in patients with chronic LBP in Kwazulu-Natal, South Africa. BMC Musculoskeletal Disord 2022;23:438, doi:10.1186/s12891-022-05397-4.
- Nicol V, Verdaguer C, Daste C, et Chronic LBP: a narrative review of recent international guidelines for diagnosis and conservative treatment. J Clin Med 2023;12:1685, doi:10.3390/jcm12041685
- Chen S, Chen M, Wu X, et al. Global, regional and national burden of LBP 1990-2019: a systematic analysis of the Global Burden of Disease study 2019. J Orthop Transl 2022; 32:49-58, doi:10.1016/j.jot.2021.07.005

Content
Author's details
Reviewer's details
General Overview of Low Back Pain, LBP (AKA, LUMBAGO)
Background
Low back pain (LBP) or Lumbago, denotes the presence of painful sensation in the lower back in varying degrees of severity and duration, which can radiate down one or both lower limbs, and may be complicated by limbs weakness, bowel and bladder voiding difficulties as well as erectile dysfunction in males. The management of LBP varies from simple physical exercises to complex low back surgeries, and the ultimate cure depends to a greater extent on the cause of the pain. Understanding the root causes of LBP and recognizing it’s red-flag symptoms, can help in early diagnosis and effective management, as well as averting some of the complications mentioned above.
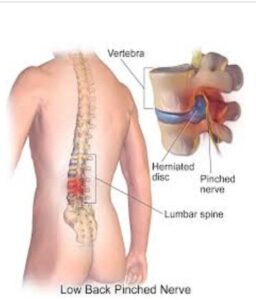
Courtesy: Physio-pedia.com/Disc_Herniation.
Further readings
- Airenakho E, Cyril OE, Blessyn OA, et Epidemiology of LBP: frequency, risk factors and patterns in South-South Nigeria. Reumatologia 2023;61(5):360-367, doi:https://doi.org/10.5114/reum/173377
- Bello B, Bello A systematic review on the prevalence of LBP in Nigeria. MiddleEast J Rahabil Health 2017;4:e45262, doi:10.5812/mejrh.45262
- Kahere M, Ginindza A cross-sectional hospital-based study of correlates of disability in patients with chronic LBP in Kwazulu-Natal, South Africa. BMC Musculoskeletal Disord 2022;23:438, doi:10.1186/s12891-022-05397-4.
- Nicol V, Verdaguer C, Daste C, et Chronic LBP: a narrative review of recent international guidelines for diagnosis and conservative treatment. J Clin Med 2023;12:1685, doi:10.3390/jcm12041685
- Chen S, Chen M, Wu X, et al. Global, regional and national burden of LBP 1990-2019: a systematic analysis of the Global Burden of Disease study 2019. J Orthop Transl 2022; 32:49-58, doi:10.1016/j.jot.2021.07.005
Advertisement

